The COVID pandemic has found a way to wreak havoc on the world in just about every way. Not to mention the astronomical impact it has had on human health, both physical and mental. One of the most prominent issues COVID has caused, besides mortal sickness, is problems with sleep.
But is insomnia a symptom of COVID-19? The answer to this is a little complicated. While insomnia isn’t a common symptom of COVID, the indirect effects of COVID, like day-to-day monotony and lack of routine, can facilitate insomnia.
The research found that 2020 saw an
increase
Trusted Source
U.S. trends in medication use for depression, anxiety and insomnia
Mental health conditions disrupt thinking, mood and behavior. From mild stress
to psychiatric illness such as depression, anxiety and insomnia, these disorders
can be a great source of distress for people experiencing symptoms, and for
those close to them.
corporate-site-labs-prod.s3.us-east-2.amazonaws.com
in the prescription of sleep medications by 14.8 percent. While the Center for Disease Control (CDC) doesn’t consider insomnia a common side effect of COVID-19, they say insomnia is common due to pandemic-related stress. As a matter of fact, insomnia many have experienced during the pandemic has been aptly deemed “coronasomnia.”
Coronasomnia is caused by a number of triggers: financial stress, emotional stress, distance from others, unpredictability, and professional concerns. Studies show that prior to 2020, approximately 24 percent of the population suffered from sleep issues. However, the pandemic saw an increase of that number up to 40 percent.
Those who are most likely to develop this unique sleep issue include COVID patients, emergency personnel, unpaid caregivers, women, and people of color. This makes sense as they have added responsibilities with little to no support.
For example, women are more likely to develop this issue because the pandemic has seen a trend in women leaving the workforce to stay home and care for their families. This ties into unpaid caregiving being another vulnerable group.
People of color Trusted Source Coronavirus in African Americans and Other People of Color | Johns Hopkins Medicine People of color are getting sick and dying of COVID-19 more than whites. A health care equity expert offers facts and recommendations. www.hopkinsmedicine.org (POC) are also more vulnerable to coronasomnia because they not only have to handle what the rest of the population is handling, but they also have systemic issues to worry about too. POC get sick with coronavirus more often than white people for a variety of reasons:
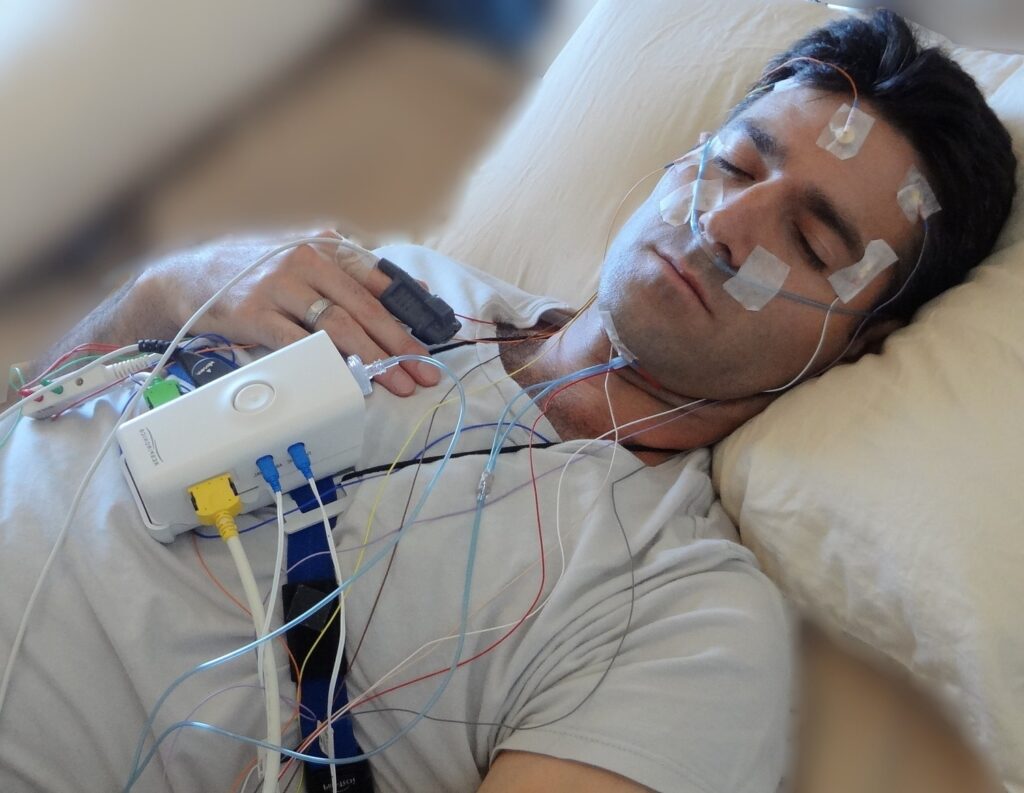
If you suspect you’re struggling with insomnia Trusted Source Insomnia - Diagnosis and treatment - Mayo Clinic Changing your sleep habits and addressing any issues that may be associated with insomnia, such as stress, medical conditions or medications, can restore restful sleep for many people. www.mayoclinic.org or other sleep issues, there are several things you can do to combat it. If you’re only dealing with occasional sleep troubles, insomnia probably isn’t the answer, but if symptoms persist for a few weeks, you should get your doctor to intervene.
Before consulting your doctor, here are a few things you could try: